Critical Review of the SIP 2024-2025 for Bangladesh’s Health Sector: Key Weaknesses and Areas for Improvement
Introduction
The Strategic Implementation Plan (SIP) 2024-2025 for Bangladesh’s health sector is intended to guide the country towards achieving Universal Health Coverage (UHC) and the Sustainable Development Goals (SDGs). However, a critical analysis reveals several weaknesses that could hinder its effectiveness. This review identifies key areas where the SIP falls short and suggests improvements to enhance its strategic impact.
1. Lack of Clear Strategies for Achieving UHC and SDGs
The SIP 2024-2025 lacks a clear roadmap or detailed strategies to achieve UHC and the SDGs. While the document lists broad objectives, it fails to provide actionable steps or policies for achieving these goals, especially in the context of post-COVID-19 recovery. There are no specific timelines, indicators, or designated responsible parties to ensure effective monitoring and evaluation of progress (pages 14-15).
Suggested Improvement: The document should include detailed, step-by-step strategies with timelines and responsible parties assigned to each action. Including measurable indicators would facilitate better tracking of progress towards UHC and SDGs.
2. Insufficient Focus on Post-COVID-19 Health Challenges
The impact of COVID-19 has profoundly affected the health sector, yet the SIP does not adequately address the strategies needed to tackle post-pandemic challenges. The plan lacks depth in addressing long-term health impacts of COVID-19, mental health issues stemming from the pandemic, and strategies to build resilience against future pandemics (pages 33, 36).
Suggested Improvement: Incorporate comprehensive strategies for pandemic preparedness and response, focusing on mental health, long-term COVID-19 effects, and strengthening health system resilience.
3. Weakness in Integrating Social Determinants of Health
Although the SIP acknowledges social determinants of health, it lacks concrete strategies to address these factors comprehensively. There is no clear plan for multisectoral collaboration to tackle issues like housing, education, and employment, which are critical for improving health outcomes (page 9).
Suggested Improvement: Develop a detailed strategy for integrating social determinants into health planning, with specific roles for various sectors and mechanisms for coordinating efforts.
4. Inadequate Emphasis on Health Workforce Development
The SIP recognizes the shortage and maldistribution of health workers but fails to outline robust strategies for health workforce development. There is a lack of specific plans for recruiting, training, and retaining health professionals, particularly in underserved areas (pages 58-59).
Suggested Improvement: The document should include a comprehensive human resource plan, detailing recruitment, training, and retention strategies to ensure a well-distributed and adequately skilled health workforce.
5. Limited Focus on Health Financing and Resource Allocation
While health financing is identified as a critical area, the SIP lacks specific strategies for increasing domestic resource mobilization and optimizing existing resources. It does not provide a clear plan to address the resource gaps for the 5th Health, Population, and Nutrition Sector Program (HPNSP) or ensure financial sustainability (pages 62, 79-84).
Suggested Improvement: Introduce a detailed financing strategy, including innovative financing mechanisms, to close resource gaps and ensure financial sustainability.
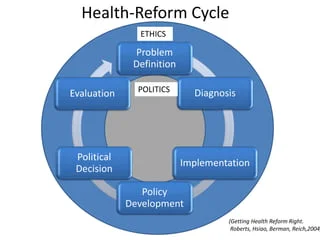
6. Absence of a Clear Monitoring and Evaluation Framework
The SIP lists several strategic objectives and components but lacks a comprehensive monitoring and evaluation framework. There is a need for specific, measurable indicators, baseline data, and clear targets to monitor progress effectively (pages 15-16).
Suggested Improvement: Develop a robust monitoring and evaluation framework with specific indicators and targets to facilitate effective tracking of progress and make necessary adjustments.
Conclusion
The SIP 2024-2025 for Bangladesh’s health sector outlines broad objectives and acknowledges key challenges but lacks the depth needed for significant improvements. To serve as an effective strategic guide, the document must provide detailed strategies, a clear monitoring framework, and address post-COVID-19 challenges, health workforce development, and health financing.
Commentary: Based on this critical review, the current SIP is unlikely to drive substantial improvements in Bangladesh’s health sector. The absence of detailed strategies, actionable steps, and a robust monitoring framework limits its potential impact. To achieve the goals of UHC and SDGs, the SIP must fill these gaps with a more detailed, actionable roadmap.