Integrating National Health Insurance (NHI) and Social Health Insurance (SHI) for Health System Reform in Bangladesh
In the context of Bangladesh, integrating National Health Insurance (NHI) and Social Health Insurance (SHI) can provide a phased approach to achieving Universal Health Coverage (UHC) while addressing the country’s unique challenges, such as high out-of-pocket expenses, low government health spending, and fragmented healthcare delivery systems.
1. The Need for Both NHI and SHI
National Health Insurance (NHI):
- Target Population: Entire population, with a focus on low-income groups and informal sectors.
- Mechanism: Tax-funded or subsidized health insurance managed by a central body.
- Purpose:
- Ensure equitable access to healthcare services.
- Address socio-economic disparities in healthcare financing.
- Provide a safety net for marginalized populations.
Social Health Insurance (SHI):
- Target Population: Formal sector employees, businesses, and their dependents.
- Mechanism: Employer-employee contributions pooled to cover healthcare costs.
- Purpose:
- Reduce financial pressure on government resources by engaging the private sector.
- Build a contributory system that encourages private sector accountability.
- Serve as a pilot for broader insurance mechanisms.
2. Why Both Are Needed Initially
Resource Mobilization:
- SHI can generate immediate funds through contributions from employers and employees.
- NHI can address the gap for populations not covered by SHI, such as informal workers and the unemployed.
Gradual Integration:
- SHI and NHI can operate as complementary systems initially, creating coverage for all population groups while refining administrative mechanisms.
System Fragmentation Mitigation:
- Both systems ensure no population group is left out during the early phases of health system reform.
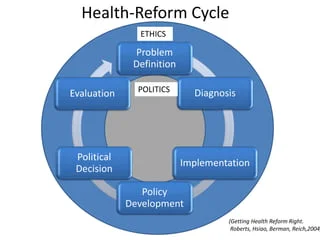
3. Implementation Approach
Phase 1: Dual System Launch
- SHI Implementation:
- Start with formal sector employees (e.g., private companies, NGOs, and government sectors).
- Mandate employer-employee contributions, managed by an independent Social Health Insurance Authority.
- NHI Implementation:
- Focus on the informal sector, the unemployed, and marginalized groups.
- Fund through general taxation, donor assistance, and earmarked funds (e.g., VAT on luxury goods).
Phase 2: Integration into a Unified System
- Governance Integration:
- Merge SHI and NHI into a single National Health Insurance Authority (NHIA).
- Introduce a unified health financing law ensuring alignment of SHI and NHI objectives.
- Cross-Subsidization Mechanisms:
- Use SHI contributions to supplement NHI funds for better risk pooling and resource allocation.
- Introduce subsidies for the poorest and hardest-to-reach populations.
- Digital Integration:
- Create interoperable digital platforms for unified beneficiary registration, claims processing, and data management.
Phase 3: System Maturity
- Establish a single-payer model under the NHIA to ensure efficiency and reduce administrative duplication.
- Expand revenue generation streams, such as mandatory contributions from the informal sector and innovative financing mechanisms.
4. Governance and Accountability
| Aspect | Proposed Mechanism |
|---|---|
| Governance Structure | Create an independent National Health Insurance Authority (NHIA) to oversee both SHI and NHI. |
| Accountability | Annual performance audits, public reporting, and grievance redress systems. |
| Stakeholder Engagement | Collaborate with the private sector, NGOs, and communities for seamless implementation. |
5. Benefits of the Dual System
- Equity:
NHI ensures access for vulnerable groups, while SHI provides tailored coverage for the formal sector. - Financial Risk Protection:
Reduces out-of-pocket spending by providing pooled resources. - Sustainability:
Combines government funding (NHI) with contributory mechanisms (SHI) for a stable financing model. - Flexibility:
Allows Bangladesh to adapt to its evolving socio-economic conditions. - Efficiency:
Risk pooling and cross-subsidization improve resource allocation and reduce duplication.
6. Challenges and Mitigation Strategies
| Challenge | Mitigation Strategy |
|---|---|
| Fragmentation of Coverage | Design a roadmap for gradual integration under a unified NHIA. |
| Resistance from Stakeholders | Conduct stakeholder consultations and awareness campaigns about long-term benefits. |
| Administrative Complexity | Use digital tools to streamline registration, claims, and fund management. |
| Limited Fiscal Space | Explore innovative financing, such as taxes on tobacco or alcohol, to fund NHI. |
| Informal Sector Inclusion | Pilot community-based insurance schemes linked to NHI. |
7. Path Forward for Bangladesh
Policy Framework:
- Enact a legislative act for the creation of the NHIA.
- Mandate SHI contributions while ensuring subsidies for NHI.
Pilot Testing:
- Test SHI in industrial hubs and NHI in rural and underserved regions.
Capacity Building:
- Train administrators, healthcare providers, and stakeholders on dual-system management.
Monitoring and Evaluation:
- Use KPIs to measure coverage, financial sustainability, and health outcomes.
Conclusion
A dual-system approach combining SHI and NHI is a feasible and effective pathway for Bangladesh to reform its healthcare financing while transitioning toward UHC. By leveraging SHI to mobilize resources and NHI to ensure equity, Bangladesh can establish a robust, sustainable, and inclusive health system tailored to its unique needs. Integration under a unified NHIA will further streamline operations, enhance efficiency, and achieve long-term health goals.