“Strengthening Primary Healthcare in Bangladesh: The Feasibility and Impact of a General Practitioner (GP) System for Equitable Health Services Delivery”
Introduction to the GP System in Bangladesh
A General Practitioner (GP) system is crucial for primary healthcare delivery worldwide, offering first-contact, continuous, and comprehensive care. For Bangladesh, the introduction of an effective GP system could significantly improve healthcare delivery, especially considering the country’s demographic and health challenges.
Why the GP System is Important for Bangladesh’s Healthcare
- Primary Care as the First Point of Contact
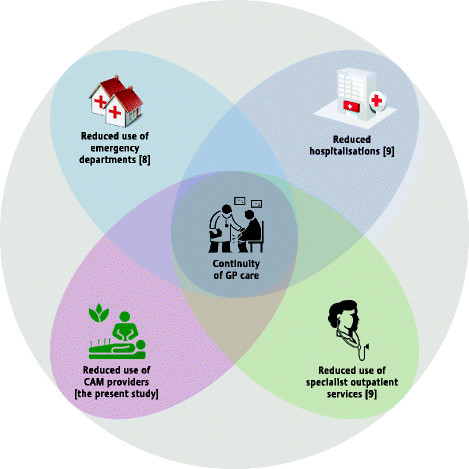
Overcrowding in secondary and tertiary hospitals in Bangladesh could be alleviated by implementing a GP system. GPs can address common health concerns and offer early diagnosis and treatment, reducing pressure on higher-level health facilities. - Continuity of Care
GPs provide long-term, personalized care, maintaining health histories and enhancing treatment adherence. In Bangladesh, where patients frequently switch providers, GPs can offer consistency and better management of health conditions. - Preventive Care and Health Promotion
A GP-centered healthcare model could improve preventive care through immunizations, health screenings, and public education, particularly in reducing the growing burden of non-communicable diseases (NCDs) in Bangladesh. - Cost-Effective Healthcare
Bangladesh’s out-of-pocket health financing model places a significant burden on individuals. A robust GP system can offer cost-effective solutions by reducing the need for expensive specialist care and hospitalizations, advancing the goal of Universal Health Coverage (UHC). - Decongesting Hospitals
A GP system can reduce patient overload in secondary and tertiary hospitals by managing common illnesses at the primary care level, improving hospital efficiency and patient experience. - Improved Referral Systems
GPs can streamline patient referrals to specialists, ensuring that only necessary cases are escalated, which helps reduce unnecessary specialist consultations and improves care coordination.
Feasibility of Implementing a GP System in Bangladesh
- Infrastructure Readiness
Bangladesh’s existing primary healthcare infrastructure, though decentralized, needs upgrading. Addressing shortages of trained personnel and medical equipment is essential to support a GP model. - Human Resources
The country faces a shortage of general practitioners. Reforms in medical education and incentives are needed to encourage doctors to pursue general practice, especially in underserved areas. - Patient Perception and Behavior
Changing the cultural preference for specialists over GPs requires public education and trust-building to demonstrate the efficacy and reliability of GPs as primary care providers. - Healthcare Financing
Reforming the health financing system to support the GP model, possibly through health insurance schemes or government subsidies, will be essential to ensure sustainable and equitable healthcare access. - Health Information Systems
Digital health platforms and telemedicine could play a pivotal role in establishing a GP system in Bangladesh by enabling efficient patient management and continuity of care. - Policy and Regulation
The government must introduce policies and regulatory frameworks to support the development of a GP system, ensuring that GPs follow standardized treatment protocols and continuous professional development.
Benefits of the GP System for Bangladesh
- Lower Healthcare Costs: Reducing hospital visits and specialist consultations can lower the overall cost of healthcare.
- Equitable Access: GPs in rural and urban areas can ensure more equitable healthcare access.
- Improved Health Outcomes: A focus on preventive care will help reduce the burden of NCDs and other diseases.
- Workforce Optimization: Efficient utilization of GPs can relieve pressure on specialists and tertiary hospitals.
- Achieving UHC: The GP system aligns with the goal of Universal Health Coverage by making healthcare more accessible and affordable.
Action Plan for Establishing a GP System in Bangladesh
- Short-Term (1-2 Years): Policy formulation, pilot projects, workforce training, and public awareness campaigns.
- Medium-Term (3-5 Years): Expand the GP system nationwide, introduce health insurance models, and strengthen referral systems.
- Long-Term (5-10 Years): Fully institutionalize the GP role, expand preventive services, and ensure sustainable funding.
Conclusion
The implementation of a General Practitioner (GP) system in Bangladesh is feasible and essential for strengthening primary healthcare delivery. By addressing infrastructural, financial, and cultural barriers, the GP model can serve as the foundation for achieving Universal Health Coverage (UHC) and improving health outcomes across the population. Public-private partnerships (PPP) and international support will be crucial for the system’s scalability and sustainability.